ike many physician-leaders, I did not choose the path of leadership with any deliberate intent. But as physicians we are leaders, whether we think we are or not. We lead care-delivery teams, we lead patients in shared decision-making, and we lead at home and in our communities. My daughter, a user-experience designer who works for a medical device company, reminded me of this recently, saying, “Mom, the doctor has the largest voice in the room, even when they’re not talking.”
cover story one
Physicians and Adaptive Change
The little med school on the prairie
By Cindy Firkins-Smith, MD, MHCI, FAADD
And change is relentless in medicine. Some of that change has been miraculous and some lamentable. In my nearly four decades studying and practicing medicine, I have seen both in spades. When I started seeing patients, I wrote clinic notes in longhand. It was not unusual to have a note consist of four lines, not much longer than the Subjective, Objective, Assessment, & Plan template of the SOAP note, which was a relatively new adaptation at the time. Reviewing a medical history could mean hunting for and digging through reams of paper charts. And after the only two-week vacation I have ever taken in my career, I returned to four to five stacks of charts — piled waist high — that I needed to navigate, review and sign.
I may complain about the burdensome clicking and pecking that is Epic, but I’m grateful for being able to put images in my patient’s note and not having to struggle to read my own illegible scribbles. Over the decades, diagnostic and therapeutic regimens have advanced far beyond what I ever envisioned. Where my options were once limited or rudimentary, now the choices abound. Where I once watched my metastatic melanoma patients die for lack of any effective treatment, many now live for years — even decades — without appreciable disease. Yet despite wider therapeutic options, I struggle to get many of those very effective medications covered, a change that I despise.
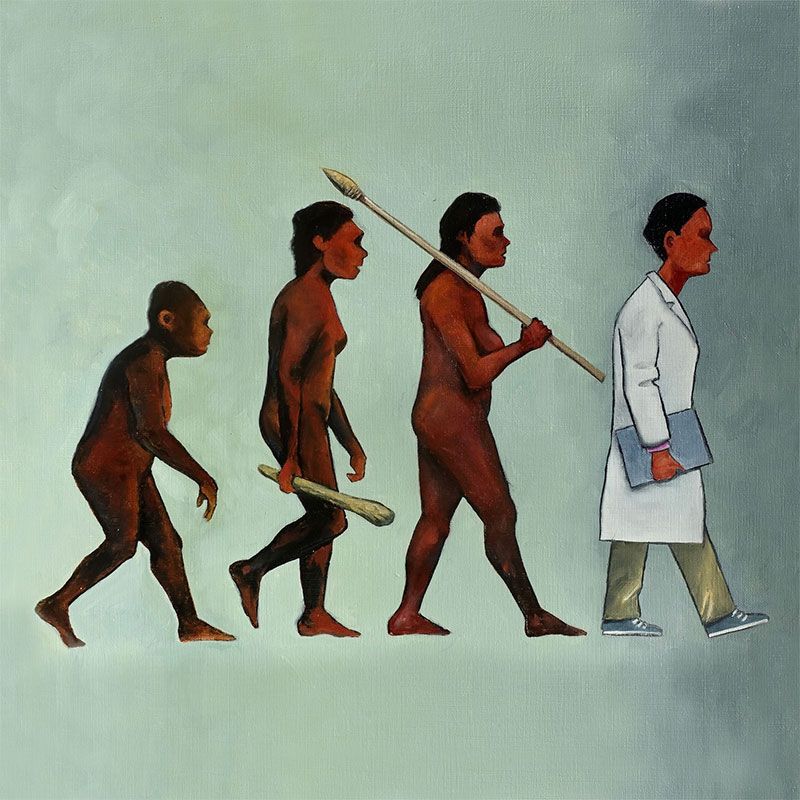
I have heard it said many times that doctors “don’t do well with change.” I challenge that. Doctors, nurses and people working in clinical settings change all the time. Everything around us is changing: drugs, insurance, protocols and of course patients. We’re trained to react and change quickly because if we don’t, people will be harmed or die. That kind of change is “technical change.” Technical changes are responses to challenges or situations that are relatively straightforward. If a drug is unavailable, we flex to what is. If a patient is decompensating, we immediately change our therapeutic approach.
It is adaptive change that challenges us. And it is not just us; adaptive change is hard for everyone. Adaptive change is required when the challenge is extremely complex, or the potential solution is nebulous, one of many options, potentially risky, and requires the collaboration and collective effort of others. Oftentimes it may compel restructuring of values, culture, attitudes and tradition. Simply put, adaptive change upsets apple carts
The doctor has the largest voice in the room, even when they’re not talking
Health Care Challenges, Fear and Loss
The health care industry is experiencing great uncertainty. The COVID-19 pandemic exacerbated a host of challenges that we now face head-on. Our health care system is built on structural and access inequity based on geography, privilege and money. Much of the health care dollar is diverted to support an increasingly expensive infrastructure. We invest massive amounts of money in caring for diseases that may have been prevented had we invested in addressing health inequities and social determinants of health. And we do not have enough people. Scores of nurses, physicians and other health care professionals left the bedside during COVID-19 and have not returned. This is especially acute in rural Minnesota where we simply do not have enough professionals to care for our people, who already suffer poorer health care outcomes related to age, chronic illnesses and geographical isolation.
I have been recruiting physicians to rural Minnesota for 33 years and it has never been harder than it is now. According to November 2023 data from the Minnesota Department of Health, the average age of a rural Minnesota physician is 59, and 1 in 3 plans to leave practice in the next five years. Rural medicine faces a crisis.
In 2016, when I became CEO of ACMC, a physician-owned multispecialty clinic based in Willmar, my partners assigned me one overriding task: map our future. This was a charge requiring inordinate adaptive change. The group had more than 115 physician-owners, another 75 or so clinicians, and 955 employees in seven different community clinics across west central and southwest Minnesota. ACMC had been a successful physician-owned organization for more than 50 years. But the winds of health care change had threatened our ability to serve our patients. Medicare and Medicaid covered more than 50% of our patients and our ability to cost shift that inadequate reimbursement to private payers was no longer possible. Shrinking revenue made it challenging to pay clinicians and staff competitive wages, and our ability to recruit physicians to our rural communities depended on our ability to pay them more than they could earn in urban areas. In more than one of our rural clinics we had not recruited a new physician for nearly a decade. We provided the bulk of primary and specialty care for much of west central and southwest Minnesota. If we could not survive, who would take care of our people?
The answer came in joining forces with our largest community hospital, Rice Memorial, and becoming a wholly owned subsidiary of CentraCare, a rural-focused health system with like-minded goals dedicated to delivering outstanding care to patients and keeping them close to home. This was beyond adaptive change for our organization; it was transformational. It could also not have been more timely. When the pandemic descended on us two years later, the collaborations born of that agreement allowed for the creation and system-wide adoption of policies, processes and care coordination that saved many lives in our region. That communication, coordination and commitment to patient safety has been expanded and continues to optimize care throughout our region.
The truth is that people in medicine, or in any field for that matter, do not fear change. They fear loss. They fear change might result in their loss of autonomy, authority, status, income, security, freedom, time or something else dear to them. When we truly seek change, we must first identify what we are asking of people, and we must understand what loss they fear. Then we must determine if the change is really at the core of that loss or if the loss is like gravity and beyond our control. And then we must ask what will they lose if we do not change?
When ACMC looked to join CentraCare, the greatest fear our doctors expressed was the loss of autonomy. And when I asked each physician to tell me what autonomy meant to them, each had a different answer. Some of that lost autonomy was long gone; the autonomy to always choose the therapeutic option we thought best for our patients had already been lost due to insurance coverage, restrictions or lack of any insurance at all. Some of that autonomy, such as the desire to attend their child’s baseball game, would not be lost, though the process to achieve it might be changed.
And what would have happened had we not changed? We may not have survived to serve our patients. We certainly would not have been able to serve our patients the way we did through COVID-19 and some of them may not have survived as well.
The Little Medical School on the Prairie
One of the most exciting health care changes taking place in our region today is the development of the University of Minnesota Medical School’s new regional campus in St. Cloud, which will welcome its inaugural class of medical students in the fall of 2025.
At CentraCare we have long had educational collaborations with academic institutions and have provided clinical rotations for students in medicine, nursing, lab sciences, physical therapy, pharmacy, respiratory therapy and many other fields. But when we looked at our numbers, we simply were not educating enough students to fill the need, especially in our rural communities.
Change is relentless in medicine.
The University of Minnesota CentraCare Regional Campus in St. Cloud started as a vision by Dr. Ken Holmen, CentraCare CEO. In 2015 he mapped the future of CentraCare and envisioned a local medical school as a vehicle for rural workforce education and expansion in western Minnesota. Though discussions had begun, like many things, they fell victim to COVID-19.
As COVID-19 demands abated, Dr. Holmen reached out to Dr. Jakub Tolar, dean of the University of Minnesota Medical School, and talks of creating a third campus of the medical school resumed. The CentraCare Board of Directors and University of Minnesota Board of Regents embraced the idea and planning began in earnest.
Dr. Holmen, Dr. Tolar and very enthusiastic and collaborative teams at both CentraCare and the university’s medical school have been working together to achieve this vision. Our state political leaders have recognized what this endeavor means to health care delivery in rural Minnesota and have contributed financial support. Our communities have responded beyond our wildest dreams with excitement and philanthropic support as well.
We’ve spoken with rural community leaders about the potential impact this campus will have on their communities, from a health, business and education standpoint. They believe it will be transformational. I have spoken with rural high school principals and superintendents, and many could not remember the last time one of their students went to medical school. Many of their students are not even going to college. When asked why, they responded, “Our kids don’t see themselves there.”
We believe that by creating this medical school campus in west-central Minnesota, where none has previously existed, our students will see themselves pursuing health care careers. We intend to create clinical exposures and mentoring for local students starting as early as grade school so they can see what they can become and get the support needed to get there. Many forget that our rural communities have strong immigrant and underserved populations that shape our cultures. We know that people get the best health care outcomes when they receive care from health care professionals that share their backgrounds and experiences. We want to ensure that our promising rural students of all backgrounds get the education, exposures and experiences they need to be successful medical students. We want to educate and train them close to home and bring them back to serve their communities.
The medical school is just one of many pieces of the University of Minnesota academic affiliation. We will create and expand residency programs to continue the education of our future physicians after medical school. We are also teaming up with the university to create a research collaboration that will bring clinical research studies closer to home, and we are also expanding our University of Minnesota clinical partnerships. All of this will improve health outcomes for our rural patients, and they will receive this care close to home.
Additionally, we are expanding educational endeavors with other collaborating colleges and universities and have recently created two new programs, one in respiratory therapy in St. Cloud, and one in radiological technology in Willmar. We believe that the medical school will create a halo effect. We know that not every rural student will choose to become a physician, but many will choose other highly needed health care careers that serve our patients.
This is a lot of adaptive change. Fortunately, we have many physicians and other health care professionals who are extremely excited about teaching and supporting our students. We have recently added physician colleagues who chose to join us because of our new academic mission and the collaboration with the University of Minnesota. We have many who are curious about what this change will bring. And we have some who fear loss, whatever that might mean for them.
How will we measure success?
Hope is never a good strategy. But if that hope is accompanied by action, it can drive change in the same ways that hopelessness breeds stasis.
The CentraCare Regional Campus in St. Cloud will welcome 24 students in the entering class of 2025. It is an investment in our future with transformed facilities that meet the needs of today’s medical students, offers a culture that champions future healthcare leaders and innovators and trains future physicians to serve rural Minnesota, where they are needed most. It expands on the rural mission of the University of Minnesota Medical School’s Duluth campus, which is working to transform its current 2-year campus to a 4-year campus.
By the time the first CentraCare Regional Campus-St. Cloud class graduates in 2029, we intend to have expanded St. Cloud residencies from our current 18-resident family medicine residency and add a 6-resident family medicine rural training program in Willmar. We are also in the process of researching funding opportunities and readiness for residency development in multiple other rural high-need areas, including pediatrics, psychiatry, general surgery, internal medicine and obstetrics and gynecology.
Success will be defined by greater numbers of rural students matriculating in and graduating from the University of Minnesota Medical School and greater numbers of physicians living in, practicing in and serving the health care needs of rural communities. We would like to move that “average age of rural physicians” number down a few years. We will define success by training more rural physicians who have lived experiences like the patients they serve and by achieving better health outcomes for our rural patients and communities.
Success will be defined by the creation of physician leaders who embrace change, not as something to fear but as an opportunity to correct the wrongs in our system; physician leaders who don’t wait for change to happen but influence change to improve the health and lives of our patients and our communities.
Hope for a better future drives this change, and the change is what will sustain health care in our rural communities. Not changing is not an option. There is too much to lose.
Cindy Firkins Smith, MD, MHCI, FAAD, vice president Medical Education and former senior vice president Rural Health, CentraCare. She is also an adjunct professor at the University of Minnesota Department of Dermatology.
MORE STORIES IN THIS ISSUE
cover story one
Physicians and Adaptive Change: The little med school on the prairie
By Cindy Firkins-Smith, MD, MHCI, FAAD
cover story two
Anatomy of a Cyberattack: The Change Healthcare incident