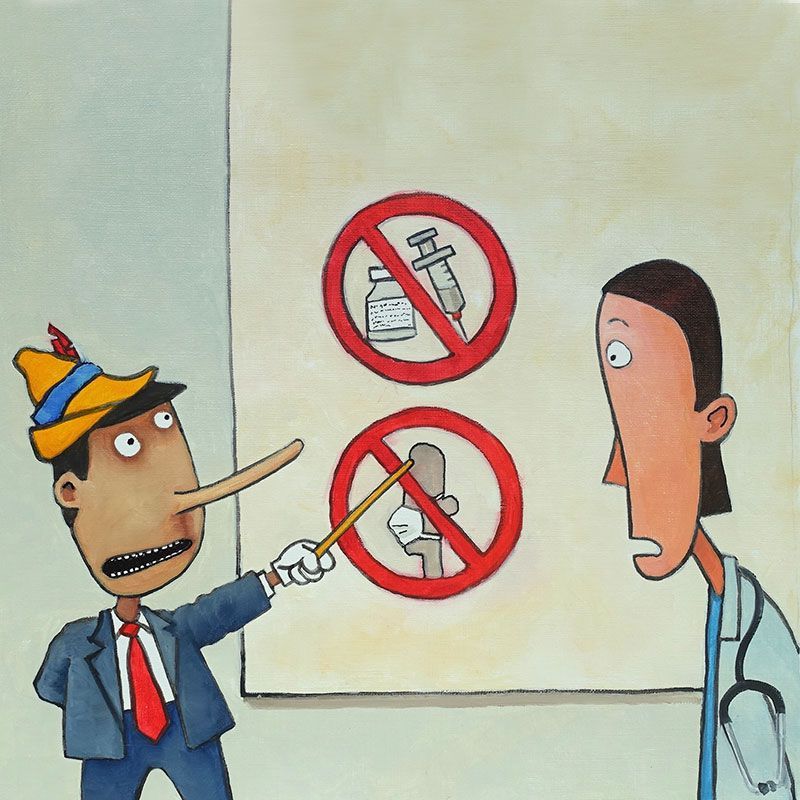
n today’s digital world, health misinformation and disinformation can spread faster than ever, often outpacing the ability to identify and provide accurate updates from reliable sources. Misinformation is defined as information that is false, inaccurate or misleading according to the best available evidence at the time. Disinformation is defined as misleading content deliberately spread to deceive people, or to secure economic or political gain and that may cause public harm. The spread of false or misleading information can erode public trust in the health care system and providers. The reduction in trust has the potential for patients to dismiss treatments, delay care or use unsafe non-evidence based alternatives. The overabundance of information including both accurate and false, also called an “infodemic,” occurs during an epidemic or crisis, making it hard for people to find trustworthy sources and reliable guidance when they need it. There is an entire science of “infodemiology” dedicated to studying the spread of misinformation. An infodemic happens when misinformation, disinformation and excessive volumes of information spread rapidly, particularly online or on social media by creating confusion, mistrust and difficulty in making informed health decisions. In regard to health care, an infodemic can amplify misinformation, distort public understanding of risks and treatments and lead individuals to reject evidence-based care, ultimately worsening health outcomes and equity.
Cover one
The Rise of Health Misinformation and Disinformation
Recognizing the Truth
By Robin Austin, PhD, DNP, RN, DC, AND Katheren Koehn, MA, RN
The History of Health Care Misinformation
Unfortunately, the spread of false or misleading health information is not new. A historical perspective can show inaccurate and misleading information dating back to smallpox, cholera, 1918 influenza and HIV. This was brought to the forefront during the COVID-19 pandemic and the rapidity of which misinformation spread during today’s digital world.
Strengthen patients’ information resilience by helping them think critically about what they see online.
Health misinformation has seen a meteoric rise for several reasons. First, the information age has flooded people with an overwhelming volume of online health content and social media posts. Second, the past decade has seen a growing decline in trust in education and professional expertise. In addition, conflicting political agendas have increasingly influenced how the public interprets and values scientific evidence. Finally, the addition of artificial intelligence and “deep fakes” further complicated the ability to discern fact from fiction.
The consequences of health misinformation extend far beyond confusion. While misinformation disproportionately harms us all, it disproportionately impacts vulnerable populations, worsening health disparities and undermining public health efforts in disease prevention (e.g., vaccinations) and chronic disease management. Current research also suggests the act of having access to valid and reliable health information is a form of equity and stresses that everyone should have access to the proper health information they need to make informed health decisions. For health care providers, understanding and addressing this growing challenge is critical to restoring trust and promoting equitable, evidence-based care.
Specifically, preventive decline in population health such as the resurgence of measles and whooping cough rates in communities with lower vaccine uptake demonstrates how misinformation leads directly to preventable illness, hospitalizations and deaths. Promoting health literacy is more important than ever, such as directly addressing misinformation about mammograms, colonoscopies or hepatitis B vaccines.
Weaponizing science refers to the deliberate manipulation or suppression of scientific knowledge to advance political or ideological agendas. This can take many forms, such as defunding research that includes diversity, equity and inclusion (DEI) components; spreading false claims about vaccines or autism; or replacing experienced regulatory experts with individuals who openly admit to having no background in public health. Each of these actions erodes public trust and undermines scientific integrity.
A striking example occurred at the University of Minnesota Medical School for a recognized medical researcher, who was conducting a federally funded cancer study that intentionally included people of color to ensure meaningful and representative data. Despite the rigor and inclusivity of their approach, the project’s funding was abruptly revoked under policies that prohibit DEI-related activities, a clear illustration of how science can be weaponized to silence equity-driven research and hinder progress in public health. Unfortunately, there are many additional examples of this in the last year across other academic institutions. The disruption of research will be felt for generations.
Gaining Control
Misinformation can worsen health disparities and inequities. Unequal access to reliable information leaves some communities more vulnerable. Moreover, when groups such as women, older adults and minorities are underrepresented in research, it perpetuates unequal outcomes. The combination of misinformation and missing data further amplifies existing research gaps and inequities.
When addressing misinformation with patients, health care providers should approach the conversation with empathy, curiosity and respect. Begin by acknowledging that it’s understandable to feel confused given the overwhelming amount of information online. Rather than dismissing or confronting false beliefs directly, invite discussion by asking where the information came from and what concerns it raises. This opens space for trust and shared problem-solving. Then, calmly provide clear, evidence-based information and direct patients to credible sources such as the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), or other major health organizations such as the American Public Health Association (APHA). By validating the patient’s perspective while gently correcting inaccuracies, providers can strengthen relationships, build confidence in science and empower patients to make informed health decisions. Every conversation is a chance to educate against misinformation, promote accurate health messages and strengthen patients’ information resilience by helping them think critically about what they see online. By staying open, patient and factual, providers can build trust and empower people to make confident, informed decisions about their health. Below are examples that can be easily adapted and provide ways to communicate with patients or community members who may be struggling with misinformation or disinformation.
Promoting health literacy is more important than ever.
- It makes sense that you’d have questions. There’s been so much conflicting information online, and you’re not alone in feeling uncertain.
- That’s a common claim online, but the scientific evidence actually shows something different. Here’s what we know from research.
- Can I show you a few ways to check if a health website or post is trustworthy?
- When you come across information like that, look for the source such as reputable health organizations like the CDC, WHO or (refer your own organization’s website if appropriate), which usually have reviewed, evidence-based content.
A cross-cutting interdisciplinary approach is needed to mitigate health misinformation. Both top-down and bottom-up strategies are required to create a coordinated, system-wide response. From the bottom up, health care professionals across all disciplines must work together to provide consistent, trustworthy information at every point of care. From the top down, health systems, professional organizations and policymakers must promote unified messaging, establish clear standards for evidence-based communication and hold industries, such as pharmaceutical, medical device and insurance sectors, accountable for transparency and accuracy.
Furthermore, health administrators and leaders should consider including addressing health misinformation as a core mission of the organization and part of larger strategic initiatives. Health systems and providers must work in partnership with community members to build sustainable authentic relationships to provide culturally tailored messaging. Lastly, a joint effort between health providers, system leaders, public health agencies and policy makers must work on large scalable digital and health literacy initiatives to build misinformation resilience.
Moving forward, health care stands at a critical juncture. We must actively counter misinformation and promote trustworthy, evidence-based communication. During the COVID-19 pandemic, for example, false claims such as using bleach to treat the virus spread rapidly and endangered lives. More recently, misleading assertions linking acetaminophen use to autism have fueled unnecessary fear and confusion. To prevent such harm, we need clear guardrails such as standards and systems that promote transparency, verify credible sources and hold individuals and platforms accountable for spreading false health information. These guardrails should balance freedom of expression with the ethical responsibility to protect public health and restore trust in science.
Efforts to counter misinformation can sometimes backfire, further amplifying false claims and drawing even more attention to them, a dynamic known as the shadowboxing paradox. The current environment makes addressing health misinformation especially difficult. Legislative efforts often face political conflict, while federal actions sometimes appear inconsistent or lack accountability, further complicating the fight against false information.
A step in the right direction is a proactive approach through legislation and policies to address misinformation. This could take the form of guidelines for online health information. One such initiative, “Health On the Internet,” also called HON Code, was a certifying organization that would review health information for individuals or organizations wishing to be independently reviewed and vetted for accurate and reliable health information. If the information was deemed accurate and reliable the website could then display the “HON code” for the public to know the website had been properly vetted and reviewed. Unfortunately, the HON code is no longer functioning due to lack of funding, unrelated to the current federal government. Additional work in this area in the form of guidelines and a standardized vetting process is urgently needed with bipartisan support, health provider input and patient/consumer health advocate engagement.
Ethical Imperatives
A professional code of ethics serves as a foundation for addressing misinformation and guiding sustainable solutions. Upholding a professional code of ethics means prioritizing truth, accuracy and the protection of people’s well-being. These values must always override agendas sacrificing health outcomes for political or personal gain. Health providers, in all specialties, can take action. For example, advocate for ethical standards and policies within your organizations that promote transparency. Foster collaborations across sectors such as partnering with public health, educators or media outlets. Work in partnership with patients to strengthen health literacy skills and build trust through empathy.
Combating health misinformation and disinformation will require a sustained commitment, collaboration and courage across every level of the health care ecosystem. The growing erosion of public trust, politicization of science and widening inequities in access to reliable information demand coordinated action. Health professionals must lead with integrity, grounding their practices in evidence, empathy and ethics, while health system leaders and policymakers must reinforce transparency and accountability. By investing in health and digital literacy, supporting equity-driven research and upholding truth as a shared professional responsibility, we can strengthen public confidence in science and ensure that accurate, inclusive, and trustworthy health information remains the foundation of care. Now more than ever we need solidarity. The future of public health, and the lives health providers strive to protect, depend on it.
Robin Austin, PhD, DNP, RN, DC is an associate professor at the University of Minnesota School of Nursing and the specialty coordinator for the Nursing Informatics Doctor in Nursing Practice program and the director of the Center for Nursing Informatics.
Katheren Koehn, MA, RN, is the executive director of the Minnesota Organization of Registered Nurses.
MORE STORIES IN THIS ISSUE
cover story one
The Rise of Health Misinformation and Disinformation: Recognizing the Truth
By Robin Austin, PhD, DNP, RN, DC, AND Katheren Koehn, MA, RN
cover story two
The Rural Health Transformation Fund: Creating a sustainable way forward