ast week, a colleague we’ll call Kelly told me that a loved one had recently undergone a procedure that had traumatized them both. Kelly grew up with a physician parent and was surrounded by physician family friends who were staunch patient advocates, trusted experts and community leaders. She is a non-physician clinician, who works on a medical team. She has had deep faith in health care for half a century, dutifully adhering to physician recommendations for everything from screening tests to surgery.
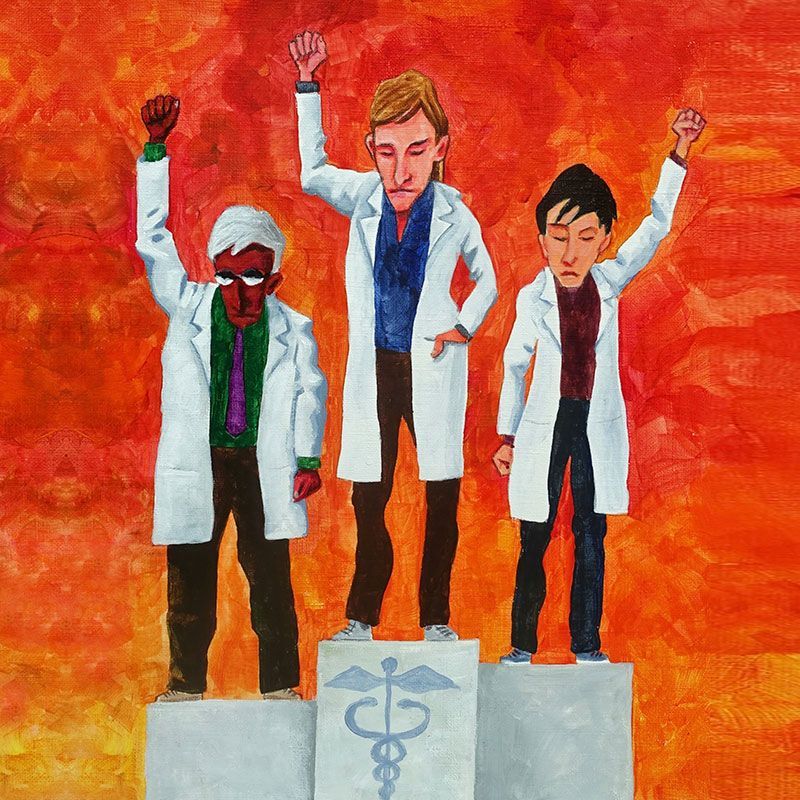
Cover one
Diplomatic Defiance
Tools for courageous leadership
By Wendy Dean, MD
But over the past five years that faith has shattered. In delicate situations, physicians have handed off care for her or her loved ones to less qualified professionals. In the most recent situation, the clumsily done — and ultimately unsuccessful — procedure cost her loved one pain, fear and something we too often ignore, indignity. And in another case, it nearly cost Kelly her life. Regretfully, she no longer believes physicians will hold their ethical line to protect patients if it puts their productivity or their jobs at risk.
Corporate capture of physicians is creating untenable conditions, and Kelly may be right. A health system in the middle of the country is in a bitter divorce with a group of contracted physicians. Administrators, with no medical training, are preparing for a catastrophic physician understaffing crisis and the consequential financial impacts to the health system by projecting redeployment of physicians to areas of specialty care they have not trained for and have never practiced. The administrators may also be advocating for and expecting the state to issue an indemnifying declaration of a state of emergency. Many doctors are yielding their ethical line, bracing to provide unsafe care. They are horrified at the potential risk to patients, are venting that horror in private online forums and feel unable to refuse — or to speak out — for fear of being locked out of employment in the health system, ensnared by a punitive noncompete clause and subsequently unable to find other work locally.
Corporate capture of physicians is creating untenable conditions.
Such stories are all too common and are a profoundly troubling illustration of the risk to clinician professionalism in the corporatized U.S. health care landscape. Physicians have been forced to learn to work effectively within the suffocating constraints of rules, policies, requirements, regulations and legislation governing their conduct. They accept those constraints in the interest of patient safety, which is sacrosanct. Those copious constraints, however, do not provide similar checks to administrators’ “innovation,” when power and finances are at stake, unless those on the inside speak out. As one physician recently said, “We just keep hoping that the cavalry is coming and they’re not.”
We are the Cavalry
This reluctance to act is not unique to health care, but few other sectors face consequences as high.
What do we do? We accept a few premises:
There is no cavalry coming and we are the ones who will “save” us. We acknowledge the inescapable moral and ethical complexity of delivering health care and the need for clarity and facility with moral and ethical principles. When our patients or our profession are in peril (e.g., we are being asked to accept a lower standard than we believe is fitting), it’s time to practice diplomatic defiance.
When I think of “diplomatic defiance” I think of 41- year-old American novelist, poet and recently named MacArthur Fellow, Jason Reynolds, and his call to “Stand on your square.” It is the steadfast refusal to be moved off the truth of our oath, off what we know is right for us — and for our patients. It is unapologetically, courageously, unwaveringly, and without drama holding our ground, our “square.” By the way, Reynolds’ interviews with Sara Enni, Krista Tippett and Brené Brown are well worth your time.
We are in an interesting moment of existential threat to the profession of medicine, in particular and perhaps slightly less so for other licensee groups. Anti-intellectualism is thriving, and the appetite for scientifically baseless “truths” about health, health care and well-being, is ravenous. Moreover, the infrastructure of “scientific truth” — reputable research institutions, respected publications, key opinion leaders unswayed by personal gain — are being torn down before us. The replacement? The collectivist truth of our new social commons: social media and artificial intelligence, where tech billionaires increasingly shape our awareness and governance through their self-serving business decisions.
Those billionaires adjudicate societal “truth” through algorithms and models, which feed content and information, respectively. But the society-wide debate about the implications of this shift is anemic. Evan Osnos, speaking on the podcast “Stay Tuned With Preet” in June 2025, argued for meatier conversations about billionaire conduct, “. . . why do we care about the lifestyles of these folks [billionaires]? Because they are reflections of values, they’re reflections of a worldview, and they’re reflections of a culture, and how we as a society expect our most advantaged, prosperous, successful people to participate in our commons.” And those billionaires have moved into health care, too, because solving its complexity is sexy (think AI) and the money flowing through the sector is staggering.
In health care, the profound shift in values has been from patient-centered or Hippocratic Oath-centered organizations to largely corporatized and financialized institutions where margin is mission. Beginning in the 1990s, health care adopted the “bigger is better” mindset, embarking on a binge of consolidation and vertical integration. Management mirrored Jack Welch-ian tenets, regardless of for-profit or nonprofit status. Only the language varied — profit or margin — but success was measured the same. Caring still gets lip service in mission statements, but those words on the walls rarely match what happens in the halls and in that discrepancy lies the root of moral injury.
When margin supersedes mission, and mission statements become focus-grouped marketing exercises, serving the margin and dissembling the public, the truthfulness and trustworthiness of those agglomerated institutions crumble. What remains, and must be salvaged from the wreckage, are the reputations of individuals who refuse to be complicit in the shift from oath-driven conduct. Retaining their ethical positions may call for, as John Lewis famously said, good trouble.
We are in an interesting moment of existential threat to the profession of medicine.
Tensions are high in a lot of health care systems as the federal government slashes research programs and threatens cuts to Medicare and Medicaid, and staff shortages are still struggling to fully recover from the pandemic. In a recent town hall meeting for a large health system, tempers flared when remote corporate executives abruptly changed scheduling platforms, making it harder for clinicians to simultaneously deliver both high quality care and high productivity. Local managers tried to reassure attendees that daily corporate emails outlining unreasonably high expectations and harsh consequences for falling short were overblown. The staff was fed up, but silent. Finally, one clinician asked a simple question in a calm, measured tone: “If that’s true, when can we expect the threatening emails to stop?”
That incisive query was a masterclass in what I am calling “diplomatic defiance.”
Defining Diplomatic Defiance
Defiance is “an act of open or bold resistance.” It is a powerful word that startles people with its directness and is loaded with negative connotations: rebellion, oppositionality, willful contrariness and disruption. Toddlers are defiant. Oppositional defiant disorder is an Axis I psychiatric diagnosis. And yet, defiance is potentially a cornerstone of addressing moral injury.
Dr. Sunita Sah, in her book, “Defy,” uses a different definition. She says, “Defiance is acting in accordance with your true values when there is pressure to do otherwise.” Between the inciting betrayal of moral injury and the transgression of one’s moral beliefs is a moment to choose whether to acquiesce to the betrayal or to speak out and push back against it — to defy. Perhaps then, “defiance” is exactly the right word for a corrective response to moral injury.
In the example of the above clinician, defiance was pushing back against bullying bosses who expected staff to work to metrics misaligned with their professional values. It is acknowledging a pressure to transgress and registering refusal to do so.
Defiance is neither a genetic endowment nor a character trait inherited from a feisty family. It is a learned and practiced skill set with the following steps:
- Know your values. Acting in accordance with your true values when there is pressure to do otherwise requires, as a setting condition, that you are clear about your values.
- Feel the threat to those values. Next, you must know the feeling of a values threat — a tight neck, a pounding heart, a knot in your stomach, an urge to flee.
- Admit the threat is happening. That inner acknowledgement is the time to plan a response — to admit to others you feel a threat, like the clinician above, or to defy, diplomatically, one hopes.
- Act. This is where practice is crucial. Accept the discomfort in defiance. The potential to create conflict is never easy and likely will never be comfortable, but it will become familiar with repetition. Repeatedly rehearsing defiant statements (or strategic curiosity, more below) puts them on the tip of your tongue in the moment. Starting early, well before a crucial moment, by practicing in low-stakes situations is essential.
What does practice look like? Being a patient in a health care situation is rife with opportunity. A few years ago, I was at a sports medicine appointment and the medical assistant “asked” me to step on a scale, with the borrowed authority — and threat of disapproval — of her boss, the physician I would be seeing. There was absolutely no need to collect that number, except to bolster billing. A hot flush announced two values threats (upcoding and putting unnecessary data in the EMR). Despite a rush of adrenaline that made me instantly nauseated, I kindly, but directly, declined. What happened? Nothing. The issue never came up in the appointment. But I’d had another chance to practice standing on my square in a low-stakes situation.
Such diplomatic defiance might also look like ending the practice of pre-appointment xrays for every orthopedic complaint or challenging anti-leakage mandates that automatically steer your patients in-house, rather than to the subspecialist who might be best for their specific case.
What about the “diplomatic” part? This is the beauty of defiance: it does not have to be rude, or loud, or bellicose. In fact, the more unemotional it is, the more effective. Diplomatic defiance is standing your ground in a way that invites others to be more thoughtful. It is pushing back in a way that makes anyone advocating for the betrayal of your professional values curious rather than defensive. Ideally, it invites others to join you on your square, because it looks like a place of clarity and safety.
Speaking Up Speaking Out
The easiest approach to diplomatic defiance is strategic and relentless curiosity, as the clinician above deployed, asking when can we expect the emails to stop? Employing diplomatic defiance to that situation could also have included asking: How does this proposed change in practice align with our organization’s mission statement? Or how can I follow this organization’s stated policy and the guidance from my professional credentialing body, if, for example, the two are in direct conflict? Or please remind me what the goal of this meeting is?
Each of us must become comfortable with diplomatic defiance: knowing when and how to speak up or push back against practices that fail to serve our patients or threaten our ability to uphold our oaths. It is a skill we can learn, and a product of values such as clarity, self-awareness, reflection, finding our voices and creating coalitions for safety in numbers.
What can you do by next Tuesday? Find a partner and start practicing some phrases, then make a commitment to low stakes practice. What about next month? Find others willing to create a coalition and decide what your common issue will be; start practicing diplomatic defiance around it. What about next year? Have a well-versed group modeling for new members and training through practice; broaden the reach of your coalition to other groups, other locations and other stakeholders (patients, community organizations, etc.).
It is time to stop walking past standards that erode the foundations of our profession.
It is time to stand on our square and lean into our professional truths courageously, holding to durable standards of empirical data, rather than expedient truths serving capricious and powerful actors.
It is time to say the things — all of them — in defense of our patients and our profession.
Leadership starts with you. Are you ready to lead courageously?.
Wendy Dean, MD, is a psychiatrist, CEO and co-founder of Moral Injury of Healthcare. She is the author of “If I Betray these Words” and co-host of the “43cc” and “Moral Matters” podcasts. She previously worked for the U.S. Army in medical technology innovation.
MORE STORIES IN THIS ISSUE
cover story one
Diplomatic Defiance: Tools for courageous leadership
By Wendy Dean, MD
cover story two
Integrating Physical and Behavioral Health Care: Solutions and benefits to the challenges